BPM brings efficiency to medical team meetings
The Grampians Integrated Cancer Service (GICS) in Ballarat is one of the nine Integrated Cancer Services (ICS) in Victoria which were established in 2004-2005 to facilitate the implementation of the Cancer Services framework for Victoria. GICS works to facilitate planning and improvements in integration and coordination of cancer services to meet the needs of people with cancer across the Grampians region.
One of the services GICS offers is the organisation of multi-disciplinary team meetings or MDMs for short. During the MDMs, the clinicians involved in the care of a patient discuss the treatment (plan) of a patient with their multi-disciplinary colleagues.
Organising the MDMs used to be a paper-based and manual process: An invitation for a MDM was drawn up based on a Word template. Once filled, this document was then faxed to clinicians or printed out and delivered to pigeon-holes. In the following week, clinicians would fill in the form and fax them back to GICS, where GICS staff would copy all the information from this form onto four other forms, which included pathology requests, radiology requests, medical history requests and surgery reports.
The manual process continued from here, as other documents such as the MDM agenda, patient list, patient data sheets and patient treatment plan forms were put together by copying and pasting data from the original form submitted by the clinician. After the MDM, hand-written treatment plans were copied and faxed to the appropriate places, leaving only a paper record for GICS.
That was the situation back in 2009. But as the demand for MDMs increased, it became obvious to Dr. Stephen Vaughan, Director of GICS at the time, that this situation was not sustainable. Moreover, valuable information on the patient was either never obtained or basically “lost”.
Clinicians tended to fill in the bare minimum of the patient information, which required lots of follow-up by GICS staff and treatment plans were not systematically recorded to allow for auditing later on. So early in 2010, Pallas Athena was engaged by GICS to help streamline the MDM organization process. The goal was to build a process-driven system that supported the organization of MDMs to make the whole process more efficient whilst also maximising the capacity of the system to capture crucial patient data.
Also, the new system would take advantage of the fact that information only needs to be entered once and could be stored for future use. Pallas Athena used the Perceptive Software Process Modelling tool that is part of the Perceptive Process suite of Business Process Management (BPM) tools to model the original process.
Perceptive Software is a global software developer of content management (ECM), business process management (BPM), intelligent data capture, and enterprise search software. The Perceptive Process Case Management software featured in this article is like a “toolbox”: It contains bits and pieces that can be put together to build a process support system.
This can include things like obtaining or writing information from/to other repositories, creating documents based on a template, integrating with other systems (e.g. mail), etc. Also, execution of these processes is by no means fixed: The user can manage exceptions to the regular process flow, as happens in everyday work, by skipping or redoing certain steps.
Through discussions with GICS staff it became clear which areas needed to be improved and what those improvements should look like. Again, this was recorded in the process model, which became the blueprint for building the process support system, which was done using the Perceptive Process Case Management software.
The initial version of the system was built over a 6 month period. It was based on the original process of organizing the MDMs with all correspondence taking place by email and all documents being automatically created, based on templates. If clinicians did not have email, the document could still be faxed or printed out. Luckily, the latter form of communication has pretty much disappeared over the last two years.
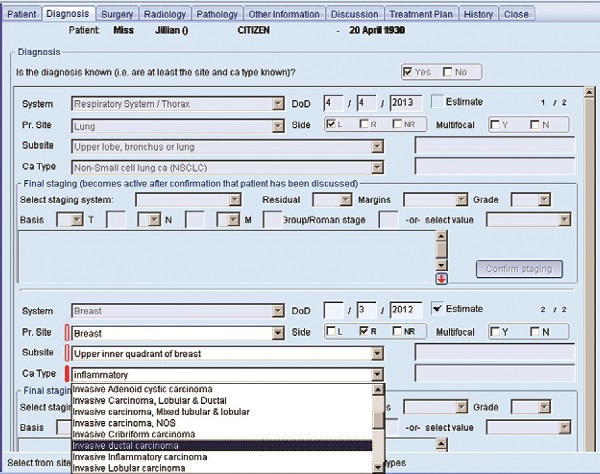
A screenshot of the MDM system. The Perceptive Process Case Management software featured in this article is like a “toolbox”: It contains bits and pieces that can be put together to build a process support system. This can include things like obtaining or writing information from/to other repositories, creating documents based on a template, integrating with other systems (e.g. mail), etc. Also, execution of these processes is by no means fixed: The user can manage exceptions to the regular process flow, as happens in everyday work, by skipping or redoing certain steps.
On the flip-side, clinicians returning documents still primarily use the fax. When the fax with the patient information comes in at GICS, a staff member still has to copy the information from the fax into the system.
To get rid of this inefficiency, Pallas Athena last year developed a web-based interface for the patient submission, called eSubmission.
“It is a rather unique approach”, explains Casper Stoel, principal consultant of Pallas Athena, “The forms in the web interface are directly based on the forms in the Case Management system. This means that if GICS wants to add or change a field related to the patient, this field automatically appears on the web interface as well. This saves time and money, as forms only have to be maintained in one place!”
Of course the implementation of the MDM system wasn’t all smooth sailing. One issue that kept popping up initially was the time commitment from GICS’ side. While the system was being developed it needed to be reviewed about every fortnight. It was difficult at times for GICS staff to free up time to do this. Later on this issue was addressed by assigning a staff member to act as an interface between GICS and Pallas Athena. This worked very well for both sides. GICS was sure that the requirements were correctly implemented and Pallas Athena was sure it was getting timely feedback on its releases.
Another issue that made the whole project challenging was the “moving target” risk. “Once a customer starts using a process support system and understands the possibilities, they usually want to add all kinds of features”, according to Stoel.
“Feedback about the functionality also led to some changes in priority. Looking back we have stretched the scope considerably, from implementing the organisation of MDMs in a process-based system, to capturing as much relevant clinical data as possible about the patient before and during the MDM. GICS has come a long way in what they are doing with the system.”
The MDM system is now fully in place and being used during the meetings to record the discussions. Louise Patterson, GICS Project Officer explains: “This has increased the credibility of the system: We are not just talking about it, the clinicians see it being used. In turn, it increases the willingness of clinicians to do their part. Now with the eSubmission the accurate submission will be mandatory for certain pieces of information, which will help to make the rest of the process run more smoothly.”
The current system contains information for over 175 completed MDMs and more than 1000 patients. It is rapidly growing now that the system is used for all the MDMs at GICS.
“We are very excited with the possibilities now that the system is live” says Bridget Wislang, Strategic Manager of GICS. “We were used to capturing just the minimal set of patient information, but now we are capturing a sizeable dataset which will help us and the clinicians in improving patient outcomes. Having all this data will allow us to track and monitor data patterns to provide feedback about the diagnosis and treatment to the clinicians involved in the patient’s care. Over the long term we will be able to provide this feedback during the MDM, which could help clinicians to make more informed decisions”.
However there is still plenty of room to expand and improve.
“We would like to see all the cancer patients in the region in the system for a full data set. Also, instead of mailing providers to request information, we would like the providers to have their own interface where they can see what information is being requested from them. Even better would be to interface directly with the pathology and radiology provider’s systems to collect the desired test results”, states Stoel.
“A first step might be to talk directly with the Ballarat Health Services’ BOSSnet system, where the majority of our patient information comes from” suggests Wislang.
She continues: “We might not have figured out yet what the next step will be exactly, what we do know is that we are going in the right direction!”
